Ozempic and others in this family of drugs are nothing short of miraculous. Meant to treat Type 2 Diabetes, the drug exploded in popularity after researchers found that patients were reporting losing 15-21% of their body weight in clinical trials. There were some side effects, but none so severe that it raised concerns. Doctors began prescribing it to people who weren’t diabetic but could benefit from weight loss, and now, our only problem seems to be getting enough of it for all the people who need it. It all seems magical, but is it too good to be true? Join us as we dive into the history of weight loss drugs, drug manufacturing regulations, and the role we think medicine should play in our lives.
Credits
Host: Alexis Pedrick
Senior Producer: Mariel Carr
Producer: Rigoberto Hernandez
Associate Producer: Sarah Kaplan
Audio Engineer: Jonathan Pfeffer
“Color Theme” composed by Jonathan Pfeffer. Additional music by Blue Dot Sessions
Resource List
Childhood Obesity in America: Biography of an Epidemic, by Laura Dawes
Fat in the Fifties: America’s First Obesity Crisis, by Nicolas Rasmussen
On Speed: From Benzedrine to Adderall, by Nicolas Rasmussen
“The NewsHour with Jim Lehrer” August 27, 1997
“NewsNight Minnesota” October 8, 1997
Oscars Monologue from Jimmy Kimmel, 2024
Transcript
Alexis Pedrick: Jerry is a scientist in his mid 40s. He and his wife have twin boys and live outside of Philadelphia. And like many people, Jerry has struggled with his weight for much of his life. He’s not quite sure when it started or what caused it, but he knows it wasn’t always this way because he has proof, pictures of himself as a 10 year old.
Jerry: And I was skinny, you know? It’s like I look very much like my kids do now to some degree, you know? Like, um and they’re eight and, um, just looking at those pictures and I’m like, okay, and then somewhere in there, all I know is when I got to fifth grade, I was five foot three and 150 pounds. Now, you know, it’s like, I’m six, two and a half now.
So I mean, I did grow more vertically.
Alexis Pedrick: But his weight kept creeping up too, until he reached 280 pounds.
Jerry: You know, I think a lot of people thought I had a look of. More of a kind of a football playing type athlete, even though I knew the truth, I’m definitely a physicist, um, you know, but reality is, you know, I’ve watched that shape still get rounder over time, you know, and even though I might have picked up some muscle, you still see the roundness and, watch my face get bigger and just saw those type of outward appearances.
Alexis Pedrick: Jerry hasn’t had a lot of time to dwell on his own self care. He spent the past couple of decades building his career and his family.
Jerry: And you work crazy hours and at some point you just look up and you just like, well, I guess this is my body type. You know?
Alexis Pedrick: Over the years, his weight would go up and down, but he always seemed to return to 280 pounds.
This was his baseline, his new normal. People of all ages, genders, and races want to lose weight for a variety of reasons. Some people want to improve their quality of life. Some people want societal approval. But Jerry’s concerns are strictly about health.
Jerry: I just kind of gave up focusing on that and focus more on just trying to be healthy as best I could, you know, and that is ultimately what really probably scared me more than anything.
Alexis Pedrick: The health aspect scared Jerry because both diabetes and heart disease run in his family, and both are associated with obesity. What’s more, studies show that excess weight puts strain on your heart, which puts you at higher risk for heart disease.
Jerry: My grandfather’s died of a heart attack when he was around my age now, maybe 43, I think it was. I, he obviously died before I ever met him or anything like that, but that was something that weighed on my father and transferred to weighing on me, you know, when it’s all said and done.
Alexis Pedrick: Over the years, Jerry tried it all. Exercise, vegetarianism, even SlimFast. Remember that? And nothing worked.
It was frustrating. Especially because as a scientist, he wanted to try something that was rooted in, well, science.
Jerry: I would love a data driven approach. All the trying things on my own and stuff and knowing that it’s led to significant bounce back if things don’t quite stay the same.
I wanted a different approach cause I mean, you can’t do this and then expect to keep gaining more weight than you lost, and expect to just keep living
Alexis Pedrick: In 2022, Jerry found his new approach through his wife, a nurse practitioner. She told him about a new weight loss drug. Maybe you’ve heard of it.
It’s called Ozempic.
Jerry: She got it and she suggested I look into it or at least talk to the weight loss doctor and I did. He came to the conclusion that Ozempic, hey, why don’t we give it a shot? And I said, why not? Even with that being said, I looked at it and even though I had a prescription in my hand, I don’t think I took it for the first maybe month that I had it.
I just let it sit there in the fridge while I kept trying to work through it cause, I was scared of it based on all of its things that were being thrown around about it.
Alexis Pedrick: Jerry had good reasons to worry. Aside from the run of the mill side effects like nausea, stomach pain, constipation, vomiting, even diarrhea, studies show that a very small number of patients (1 percent or fewer) developed more serious gastrointestinal problems, including biliary disease, pancreatitis, bowel obstruction, and stomach paralysis.
But there’s also a more serious reason to worry. It’s not an exaggeration to say that the history of weight loss drugs is very bad. And there has arguably never been a successful one. Over the past 100 years, weight loss drugs have promised miracles, but instead have been proven ineffective at best and killed people at worst.
It’s kind of a pattern. When they’re first discovered, they’re lauded as breakthroughs. And then, we find out that they’re dangerous and discard them. But the search never ends. So, the question is: is Ozempic different?
From the Science History Institute, I’m Alexis Pedrick, and this is Distillations.
Chapter One. Glands.
Throughout most of history, obesity was not considered a problem. In fact, it was the opposite. Voluptuous bodies were desirable. They were status symbols, signifying wealth and abundance. If you were curvy, it meant you had plenty to eat and you weren’t toiling in the fields. You were relaxing and being waited on.
But all of this starts to change in the late 19th century, and it coincided with the emergence of a new field of science.
Laura Dawes: In the 1890s, the kind of cool area of medicine was endocrinology.
Alexis Pedrick: This is Laura Dawes, a historian of science and author of “Childhood Obesity in America: An Epidemic.”
Laura Dawes: So in the way that genetics is the cool area now, or your microbiome, in the 1890s, endocrinology, that was it, that was the frontier of medicine.
Alexis Pedrick: Quick aside about endocrinologists. They study hormones. These are the chemicals that are pumped throughout your body by glands like the pituitary and the thyroid. And these hormones are responsible for the size and composition of your body. They control how big your bones grow and how much energy you metabolize.
The field of endocrinology became all the rage when they found a cure to a condition called cretinism.
Laura Dawes: Now, I know that today that the, that is used as a kind of a derogatory term, but it is actually a medical term referring to somebody whose thyroid is not putting out enough thyroid hormone, and their growth and their mental development has been affected because of that.
Alexis Pedrick: Cretinism prevented people from developing physically and mentally. They had swollen abdomens, their tongues were big, and adults with the condition were sometimes as short as 2 feet 8 inches.
Laura Dawes: And so in the 1890s they discovered that feeding cretins with raw sheep thyroid gland would replace that thyroid hormones that their bodies weren’t making normally.
And the results were absolutely dramatic, you know, just astonishing, really quite miraculous.
Alexis Pedrick: The patients became less swollen, their tongues returned to normal sizes, and they grew in height.
Laura Dawes: And those kinds of dramatic changes really made endocrinology and endocrinologists super excited about the possibilities for their field.
So it didn’t take too long for endocrinologists to sort of think, huh, we know that these chemicals are interfering in or controlling the shape and composition of the body. So let’s have a look at obesity and overweight, because that is a condition characterized by, you know, the large shape and high fat composition of the body.
So yeah, it was kind of almost like a specialization looking for something to treat.
Alexis Pedrick: And the timing was perfect, because by the 1920s, thin was definitely in.
The Flapper Story: It is the dawn of the 1920s. She is about to take flight. A social rebel in a short skirt and rolled stockings. A defiant champion of a new womanhood.
She will be called a flapper. This is the flapper story.
Alexis Pedrick: You’ve seen pictures of flappers. They’ve got short hair, short dresses with fringe, and they’re always, always thin, right? At least that’s what the magazine showed. In this era, eating disorders were rampant. The recent desire to be thin coupled with the discovery of glands as a treatment for weight loss: it was a potent combination and it led to a theory that being overweight was a matter of hormones being out of whack.
Laura Dawes: It’s always been very appealing, um, to patients and doctors to be able to say, uh, you do avoid the stigma, I suppose. You know, that it isn’t, as you say, a moral problem or a failure of lack of will or just being greedy.
It’s none of those things. There’s something going wrong in your body, and we can tell that there’s something going wrong in your body because we’ve got a pill. That will reach into your body and change that and, you know, fix it for you. So that’s also a really powerful element of appeal to these drug treatments for obesity.
Alexis Pedrick: And the best part about this is that they’ve worked. At least on the face of it. We don’t have exact numbers of how much weight people were losing, especially when they ingested the thyroid hormone, but the results were good enough that people kept buying them. And these drugs came in all sorts of weird forms.
Laura Dawes: So patients were being prescribed just all kinds of different gland extracts, thyroid gland, pituitary gland, mixtures of gland extracts, sometimes some really exotic kinds of ones, extracts of testicles, extracts of memory glands.
Alexis Pedrick: Sometimes they were given in ways that we recognize today, like in tablet form, but sometimes they were blended down into a pink liquid or given whole with anchovy paste to mask the taste, which really points to people’s desperation for weight loss. And endocrinologists were more than happy to oblige.
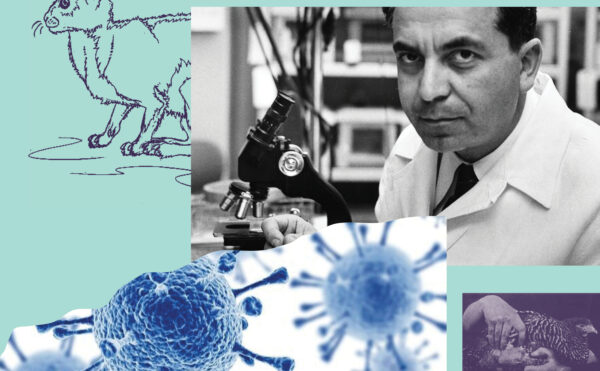
This is Nicolas Rasmussen, a historian of science and the author of “Fat in the Fifties: America’s First Obesity Crisis.”
Nicolas Rasmussen: People would joke in the 1920s that endocrinology is the specialty of making fat ladies thin.
Alexis Pedrick: But it wasn’t just medical doctors who were in on this. When there’s desperation and money to be made, con men are not far behind. One of the most notorious miracle gland tablets was called Marmola. It was made of one part desiccated thyroid, a little seaweed, and a lot of laxatives. Marmola was the creation of a man named Edward Hayes, whose previous accomplishments included making tablets for male insufficiency. Hayes, it should be said, was not a doctor. He was an opportunist.
This is John Swann, a historian at the FDA.
John Swann: His company advertised heavily in print and radio when that became available, then had his own radio show, and, you know, people flocked toward it. And, you know, it was a, it was a pretty potent medicine itself.
Marmola Entertainers: Sure, when I was a slim young thing.
Alexis Pedrick: This is an advertisement for Marmola. A woman named Connie is trying to impress her old college fling with her weight loss.
Marmola Entertainers: Well, do you happen to know that right now I weigh exactly the same as I did then? What? Just the same. One hundred and ten pounds. But you said you stopped dieting.
Right now you’re eating everything in sight. Modern women don’t go on diets. Not if they have any sense. Besides, this never did me much good. I’ll say it didn’t.
Alexis Pedrick: The biggest concerns around Marmola revolved around two things. One, the man who peddled it, Hayes. He was known as a quack to authorities. And two, the claim that the tablets were created using, quote, the latest science.
Marmola Entertainers: Connie was wise. She knew that a starvation diet was ruining her looks and sapping her vigor. But she is typical of the modern woman, who looks into the cause of things. And there is a cause for excess fat. Modern science has discovered it, and now doctors fight this cause with the right method. The results?
New beauty, new slenderness, new vim. They are seen everywhere you look. Marmola prescription tablets, prepared in a famous medical laboratory to fit the average case, present this right way to reduce at its best.
Little girl, you’re the one girl for me.
Alexis Pedrick: At this point, maybe you’re wondering, did it work? Like, it had to work at least a little bit, or no one would have ever taken it, right?
Well, for one thing, one of Marmala’s ingredients was, like we said, a laxative. And they used a lot of it. But there was another reason these gland treatments did, in fact, result in weight loss.
Laura Dawes: It will make you lose weight, particularly thyroid hormone. Not so much because it is targeting a biological problem that’s causing the obesity but because thyroid, having too much thyroid hormone causes hyper-thyrotoxicosis.
So you’re basically being poisoned by having too much thyroid hormone.
Alexis Pedrick: By the late 1920s, several federal government agencies like the Postal Service, the Federal Trade Commission, and the Bureau of Chemistry, which was the precursor to the FDA, were alarmed by how shady characters like Edward Hayes were Introducing such potent drugs to the market.
In 1926, the post office went after him because Hayes was sending his drugs through the mail, but he found a workaround. He started sending his tablets directly to pharmacies. And that’s when the Bureau of Chemistry tried to step in, but they could only do so much.
This is John Swann again.
John Swann: All they could do was publicize these problems, and they did.
Alexis Pedrick: There was actually a traveling exhibit called the “American Chamber of Horrors” that the FDA, as it was now known at this time, put together in the early 1930s to convince Congress and the public of the need for a new law.
John Swann: Marmola was a poster child in the in the Chamber of Horrors exhibit.
Alexis Pedrick: But it wasn’t until 1938 that the FDA finally had the enforcement tools to put an end to Marmola and other drugs like it.
That year, Congress passed the Drug and Cosmetics Act, which gave the FDA the authority to go after quack medicine. This put an end to charlatans selling thyroid, but we were back to the drawing board about the cause of obesity. So, we got new, but still harmful drugs. But as we’ll see, some people don’t really care how something works.
Or even if it poisons them. As long as it helps them lose weight.
Chapter Two. Amphetamines.
Smith, Kline, and French was a pharmaceutical company in Philadelphia. In 1932, they received a patent for amphetamines. Their first drug was benzadrine, which hit the market in 1934 as a decongestant. Now, amphetamines are uppers, which means they make you feel awake, uh, euphoric.
And because of this, they were repurposed in 1937.
This is Nicolas Rasmussen again.
Nicolas Rasmussen: It’s first major indication is for depression. Amphetamine has a lot of, uh, you know, mood effects, right? And it’s a breakthrough drug. It’s the first antidepressant that’s being called that by the 1940s in, in amphetamine marketing.
Alexis Pedrick: Smith, Klein, and French had a blockbuster drug and the money was flowing in. Things were going great, but then they started to notice something.
Nicolas Rasmussen: Hey, someone’s cutting into our, our sales here because the sales curve is going up and up. And then in 1930, 1940, it starts to flatten before the war. And they, they, they find out that there’s patent infringers selling amphetamine for weight loss.
Alexis Pedrick: They were being undercut by sleazy operators, phony drug companies, and so called “fat doctors.” And I hope you can hear those quotation marks, because while they were technically certified doctors, their standards for evidence were not what you’d expect today.
Nicolas Rasmussen: The “fat doctors” are often what other doctors call them because they’re, they’re not, perceived as reputable in the medical profession.
They have a clinic, they often have, some diagnostic procedures which are frequently hocus pocus. You know, they might measure your fat body mass or do something to purportedly measure, you know, your metabolism, this kind of thing to justify whatever it is they’re going to do. Um, but whatever it is they’re going to do always ends up being dispensing diet pills.
That’s how they actually make their money, not just from the patient fees. So they’re acting as the pharmacist too.
Alexis Pedrick: They were known by doctors and patients as rainbow pills. Why rainbow pills? It was all about marketing and making themselves seem like legitimate doctors.
Nicolas Rasmussen: They do their best to insulate the patients from the fact that they’re seeing 200 patients a day.
They see the doctor for only a couple minutes and nothing’s gonna, hide that from them. So the practitioners feel the need to reassure the patients that they’re getting well thought through individualized treatment. And so the doctor, when they finally see the patient will say, well, you know, the nutritionist that you’ve talked to earlier, Lois says this, and my nurse says that, and based on the results of these tests here, looking at some bogus piece of paper. I would say that, you know, you’ve got this and this, and it would be a completely irrational explanation, right? That having to do with heart failure. They had some, like, they live in a parallel medical universe, some of these guys. Anyway, they give the explanation and they say, you definitely need these blue ones, it’s a special formula.
Take, you know, one in the morning, one after lunch, don’t take one at night, take a, you know, one of these white ones instead. So, it’s a, it’s an individualized prescription, and they walk out, and then they’re likely to see someone they know. Maybe from a diet club, or maybe just because it’s a small town, and there’s only, you know, one or two of these, these clinics.
And that person that they know will say, Oh, you’ve seen Dr. Jones as well. And, yes, and I’ve got my special prescription. It’s, you know, uh, two blues, a pink and a white. And he’s like, Oh yeah, so I’ve got, I’m getting three pinks, a green and, uh, you know, and, and no white. So, oh, well, he’s so clever.
So if they don’t want to be showing basically admitting the true nature of their business, which is just cranking out these prescriptions.
Alexis Pedrick: Now, again, you might be wondering, did it work? What even was the so-called scientific reason amphetamines caused weight loss anyways? And there are a few theories.
Laura Dawes: One was that the amphetamine was influencing the hunger center in your brain. This is the hypothalamus. It’s a part of your brain at the back of your brain, which kind of receives signals from your body to know about, uh, when to metabolize fat stores and when to store them. And the idea was that amphetamines were affecting that part of your brain and kind of telling it, we’re full, we don’t need to eat.
So here it was kind of acting as an appetite suppressant in that kind of way. And so the idea was, well, maybe what is, what it’s doing is it’s making people feel happy. Um, so they don’t need to eat to feel happy. They don’t need to find pleasure on their plate anymore, um, because they can find it in other kinds of ways.
And related to that, the theory was also, well, you know, if you’re feeling happy and confident, well, then you’ve got the kind of the backbone to take on the calories. You can diet. You’re feeling all kind of pepped up and powerful.
Alexis Pedrick: Smith, Klein, and French wanted in on the craze. It was their drug after all, and other people were making money off of their patent.
So, they did two things. The first was that they created their own amphetamine weight loss drug.
Nicolas Rasmussen: So they go great guns into marketing it for weight loss in 1947. And they build the market extremely rapidly. And it’s the very same drug they’re selling as an antidepressant.
Alexis Pedrick: The second thing they did was sue amphetamine drug makers, and they won.
No more rainbow pills, right? Well, not exactly. The patent infringers just swapped out the amphetamines for something a little bit different.
Nicolas Rasmussen: Methamphetamines out there too. Clark and Clark, the biggest infringing firm, immediately switches their rainbow diet pills. They take the amphetamine out when they lose the case and put methamphetamine in.
Alexis Pedrick: So now, not only is Smith, Kline, and French being undercut by methamphetamine, but their patent for amphetamine is going to expire in 1949.
Nicolas Rasmussen: So how are they going to keep that domination when the other big drug firms are able to legally sell amphetamine? Well, partly it’s the brand, but they create a new product with greater sticking power.
And by sticking power, you could cynically say it’s a combination of two products that are both addictive. The amphetamine and the barbiturate, um, sodium amytol. This is the product Dexamyl. It’s sold as an antidepressant, but it really takes off as a diet drug. Its sales take off enormously in 1950. It becomes the firm’s most profitable product.
Alexis Pedrick: By the 1950s, a certain German cycle analyst was making waves in the US. That’s right, Sigmund Freud’s theories were now all the rage. Freud thought that the need to constantly have something in one’s mouth resulted from being stuck in an early developmental stage. He called this oral fixation. Now Smith, Kline, and French wanted to craft a narrative that obesity was a disease of the mind, not the body, because they were trying to find a new market for one of their existing drugs.
So, they sponsored a study that explicitly linked obesity to Freud’s theories.
Nicolas Rasmussen: Amphetamine is a famous psychiatric medication, okay? At the same time, the doctors are now accepting that obesity is a psychiatric condition. So, it’s doubly appropriate, right, to sell it as a weight loss drug. It treats the overconsumption of food, it suppresses appetite, that’s the official reason why it’s approved as a diet drug, amphetamine, but it also treats the underlying psychiatric condition that is often responsible for the overeating in the first place.
So that has to be related to depression. They sponsor some studies, some experts to, Smith, Kline and French does, to make that link, that the oral fixation, you know, in the depressed individual is often expressed as overconsumption of food. They have a psychiatric medication already, and so it’s perfect in this environment to market it as a weight loss drug.
Alexis Pedrick: For all this fierce competition, and the lengths Smith, Klein and French went to, people eventually noticed amphetamines didn’t even work that well. The actual weight loss with them was quite modest, just a pound or two a week, which is about what someone could achieve with a diet and exercise alone. And then it kind of plateaued.
It wasn’t such a great return for the risks. They were highly addictive and dangerous, even lethal. In 1968, a journalist, Susanna McBee, did an expose for Life magazine.
John Swann: She used her own name, uh, explained that she wanted to lose a few pounds, even though she herself was, stood 5’5 and weighed 123 pounds. She went into the clinics and even though, you know, a few of the doctors said she really didn’t need to lose weight. She still walked away with bundles of rainbow pills from each one, and so she wrote about this. It was a cover story in Life in January, and she wrote about her experience. She wrote also about some of those patients who had died taking rainbow pills, most of whom were women.
Alexis Pedrick: This led to congressional hearings, which compelled the FDA to act. They conducted mass raids on manufacturers of rainbow pills which essentially shut the supply for fat doctors. They also made amphetamines a Schedule II drug, meaning they were considered dangerous, which made it harder for doctors to prescribe them.
John Swann: Seizing pills literally by the millions, within a couple months they had seized, gosh, nearly 45 million of these tablets.
Alexis Pedrick: The final nail in the coffin of this era was none other than Richard Nixon.
Public Enemy Number One: America’s public enemy number one in the United States is drug abuse. In order to fight and defeat this enemy, it is necessary to wage a new all-out offensive.
Alexis Pedrick: This might have put an end to the rainbow pill era, but it wasn’t the end of amphetamines being used in weight loss drugs. They went away for a while and then came back in full force in the 1990s.
Chapter Three. Fen Phen
Fen Phen Song: What are the pills that cure the dieters ills by making them lose weight? Fen Phen! What do they grab in hopes of shedding the flab from all the food they ate? Fen Phen!
Alexis Pedrick: When I hear the word Fen Phen, I immediately think scandal. Uh, that’s probably because I was a child in the 90’s and it made a lot of tabloid headlines.
Fen Phen was a short-lived diet drug that was actually a combination of two amphetamines: fenfluramine and phentermine. It was popular, there were 18 million prescriptions in 1996. But also risky.
In the summer of 1997, the Mayo Clinic sounded the alarm about how dangerous it was.
The NewsHour with Jim Lehrer: Today, my colleagues and I from the Mayo Clinic report a new clinical observation of a possible relationship between heart valve disease and Fen Phen. To date, five of these patients have required open heart surgery to repair or replace damaged leaking heart valves.
On the day of the Mayo Clinic press conference, the FDA issued a dear doctor letter, warning of Fen Phen’s possible risk for heart valve disease. The letter reminds doctors that the FDA has never approved the Fen Phen combination.
Alexis Pedrick: There was another amphetamine derivative weight loss drug called Redux that was supposed to be safer than Fen Phen, but this turned out to not be the case.
Redux had the same side effects of and most serious of which was pulmonary hypertension. So, did drug makers go back to their labs and try to make a safer alternative? No. They tried to change the stakes.
The NewsHour with Jim Lehrer: There are 8 to 10 million Americans who have adult onset diabetes and who are obese and who are going to lose their limbs or their eyes or their hearts or their lives if we don’t get weight off them now.
Alexis Pedrick: This is Richard Wurtman, the developer of Redux, on The NewsHour with Jim Lehrer in 1997. He went on the show amidst the controversy to defend his product.
The NewsHour with Jim Lehrer: So I’m frankly upset about the fact that the scaremongering about nonexistent side effects of Redux has kept a lot of people who really need this drug from taking it.
Alexis Pedrick: His message was this: the real killer is obesity. Now up until this point, obesity was a medical concern, but not thought of as a disease in and of itself. But just like Smith, Klein, and French repackaged obesity as a psychological condition, a symptom of depression, Richard Wurtman wanted to label obesity as a killer, because if the alternative is death, then some risky side effects don’t look so bad.
It’s a familiar line of defense for the weight loss drug. When the drugs are being considered for approval or when they come under fire, they’re touted as lifesaving. But when the drugs are being marketed, they’re touted as a lifestyle. Drug companies want to have their cake and eat it, too.
The NewsHour with Jim Lehrer: But as critics point out, some doctors in diet clinics market appetite suppressants not just to the medically obese, but to anyone who’d like to lose a few pounds.
Dr. Rubin says one out of four patients he treats for diet drug related PPH are minimally, if at all, overweight.
There’s no magic bullet. Um, but, there is Russian Roulette and, uh, Russian Roulette is taking pills that have a substantial and to some extent not fully quantified risk when the benefits are cosmetic.
Alexis Pedrick: Part of the problem was that these drugs were intended to be taken for no more than three months. But a lot of people went ahead and took them longer. Some doctors were prescribing them for long term anyway, which left them vulnerable for malpractice suits. And patients themselves didn’t seem to care how the drugs worked or how bad the side effects were.
They just wanted to lose weight. This is a patient who was interviewed by a public TV show in the 90s.
NewsNight Minnesota: You know, you just reach a point where you’ll try just about anything. And I was there and I did a lot of research before I even went into the clinic. I, uh, we got some things off the internet and I read everything I could get my hands on.
And at the, at that point, it seemed like this, a smart thing to do. Until you heard about the ramifications of taking Fen Phen, what went through your mind? It wasn’t so much of geez, I could die. It was, gosh, what if they take it off the market? And that’s serious. That was my first reaction. It’s, you know, this has been so good for me and I do feel fine.
I still feel fine. Um, it was more, please don’t take it off the market till I’m done.
Alexis Pedrick: Fen Phen and Redux were ultimately taken off the market and thousands of lawsuits were filed against the makers of the drugs. It turns out that the drug company was withholding information from the FDA about the risks.
But the drug’s narrative arc illustrates the definitive pattern for weight loss drugs.
Nicolas Rasmussen: There’s a well-known life cycle of drugs that, you know, they’re given a hero’s greeting, you know. Successfully marketed blockbusters are first introduced. They’re going to be so much better than any other drug that’s ever come before. They go into mass use, and then because they’re being taken by millions of people, their side effects become evident, their adverse events and so forth.
Then, they go through a period of negative evaluation. Medicine, like, thinks badly of these former brilliant new drugs. And then, if the drug hasn’t been pulled off the market, like most of these that we discussed have, there comes a kind of a rational use. That’s the standard concept of the life cycle.
There’s a joke that goes with it among doctors, you know, that you should always prescribe the latest drug while it still works. You know, there’s this, there’s kind of like a social placebo effect, you know, that drugs are thought to work because they’re new.
Alexis Pedrick: And of course, now we’re at the beginning of a journey for a new weight loss drug.
Oscars Monologue: Ladies and gentlemen, your host for this evening, Jimmy Kimmel. You look great. Everybody looks so great. When I look around this room, I can’t help but wonder, is Ozempic right for me?
Alexis Pedrick: Chapter Four. Ozempic.
Weight loss drugs in the past often made claims that there was one cause of obesity. For endocrinologists pushing gland cocktails, it was a hormone imbalance.
For Smith, Kline, and French pushing their antidepressants turned diet drugs, it was a Freudian psychological problem. We seem to have at least finally admitted that there is no one simple explanation for what causes obesity.
This is Andrea Coviello, the director of medical weight management at the University of North Carolina.
Andrea Coviello: There are some genetic susceptibilities. So certain people are going to be more prone to weight gain, but then there are significant environmental influences that also stimulate weight gains. There’s trends with aging in general.
Alexis Pedrick: And hormones also play a part. For example, women often gain weight during pregnancy, while breastfeeding.
And what all of these factors have in common is that none of them can be treated with a drug. But one contributing factor to obesity, just one, involves the hormones in our guts, and that’s what Ozempic targets.
Andrea Coviello: Ozempic is one of the new class of medications that we commonly refer to as incretins, at least in the scientific community.
And incretins in general are gut hormones that you secrete from your gut, the stomach intestines, large intestines, after you eat. You release this cascade of gut hormones that then help you metabolize what you ate, but also signal the brain that you have had a meal or a snack or some food. And that stimulates your appetite regulation pathways.
So there’s a natural daily rhythm to hunger and satiety. And many of the signals that trigger hunger and satiety on and off are these gut hormones.
Alexis Pedrick: It’s important to note that a huge difference between Ozempic and historical weight loss drugs is that the entire landscape of medicine and safety regulations has changed.
The FDA, as we know it, didn’t exist yet when glands were poisoning patients. Meanwhile, while Ozempic seems like an overnight success story to most of us, it’s actually been around for more than a decade.
Andrea Coviello: So, from a healthcare perspective, they’ve been FDA approved for 15 years, right? So in order to be FDA approved, a lot of work has gone on across many years before the FDA will actually approve a new medication for use in the public.
So the actual experience with these drugs is, you know, around 20 years.
Alexis Pedrick: Still, because Ozempic began as a diabetes drug and only recently got approval for weight loss, Laura Dawes thinks we should be cautious.
Laura Dawes: These are very, very recent drugs, these ones. They’ve only been approved for use for weight loss from 2021 for Wegovy, so very, very recent.
And often the long term impacts of these things only kind of come out after time.
Alexis Pedrick: And she points out something that Ozempic has in common with so many other diet drugs. Something risky.
Laura Dawes: People are taking them for less severe versions of the condition. They are powerful drugs.
They are very powerful drugs. They are affecting fundamental processes in the body. So, we do need to be extremely cautious about drugs like that, and be very well aware of the fact that, you know, they are doing these very, very profound things to bodies. And I think that the wave of enthusiasm for them, perhaps doesn’t reflect an understanding of just how strong and powerful a drug these are.
Alexis Pedrick: When we met Jerry at the beginning of the story, he was clear that his reasons for considering Ozempic were serious.
Jerry: With me being a larger man and knowing I had an uncle that died at 50, when he was actually a larger man on that same side of the family. He died of a heart attack doing one of my favorite activities, playing cards, you know, at a card table. He was just gone.
Alexis Pedrick: He was concerned about side effects, but ultimately, he decided that the benefits outweigh the risks.
Jerry: Adverse health outcomes have been monitored in those situations, and people felt like they had a good feel on what those things were and how to mitigate them if they appeared. And ultimately, you know, determined that a lot of these side effects, or like I said, adverse health outcomes, they were all manageable, you know?
Alexis Pedrick: One month after getting the prescription, he started taking Ozempic.
Jerry: And eventually I took it, and that began in November of 2022. My gosh, it’s been, yeah, it’s been that while, like November of 2022. So I was able, due to the drug, to basically, it was probably, May, I think I got it all the way down to like 192 pounds.
Rigoberto Hernandez: Whoa.
Jerry: Yeah, go figure.
Alexis Pedrick: It was a remarkable transformation. In a period of six months, Jerry, who had never before been able to shed any meaningful weight, lost almost 90 pounds. He reached his target weight of 190 pounds down from 280. And once he did that, he reduced his dosage threefold, and he actually gained 10 pounds back.
And this is one of the drawbacks of tech fixes. They don’t actually change anything that lasts when you stop the drug. When you stop or reduce the drug, things go back to how they were.
Andrea Coviello: The concerning thing is that if you successfully lose weight with these medications and changes in your lifestyle, that if you go off the medication, you will likely gain weight back.
And it looks like maybe on average 50 percent by a year’s time or a year and a half. Some people will gain more than that back to their original weight over time. And, and that’s concerning.
Alexis Pedrick: And here lies the final big difference between Ozempic and the things that came before it. We actually define obesity differently now.
We call it a disease, a chronic disease.
Andrea Coviello: So we think of it like hypertension, high blood pressure. If you take medications for high blood pressure and you get your blood pressure down to goal, everything looks good. If you stop those medications for the vast majority of people, that blood pressure is going to go back up.
And so we think about the same thing is true of diabetes, and we think about obesity now as in that same category. If you have an effective regimen, and then you stop that regimen, and if it includes a medication that you stop, you will gain the weight back, and then likely, whatever obesity related chronic conditions that you also had will also come back.
Alexis Pedrick: Jerry says that he’s ready to take Ozempic for the rest of his life. He’s always seen weight loss as a lifetime struggle, which is why he will continue to use that tool for life.
Jerry: I have no choice because of my family history of people dying young. And also just consequences of morbidity, you know, like I don’t need a bunch of years that aren’t good either.
You know, I don’t want that as an outcome. I’m going to be forever conscious of this. This is my fight. This is my fight. I just haven’t had this much success before. And I want to hold on to that.
Alexis Pedrick: Laura Dawes says that at least today we’re more honest with ourselves, that our lives are not conducive to maintaining a healthy weight.
Laura Dawes: I think that that is a, uh, a realistic recognition that the environmental effects on us and the way that we work and the way that we live, it really does not support, uh, weight loss. And in fact, it’s actively against it in some cases, you know, the marketing of food and the types of food that are readily available to us.
So I think recognizing that you’re kind of in a losing position from the start against that environment is realistic, and it’s a good sort of first step. I would like to see that, in the future, transferred to actually making changes to that environment. Making changes to the ways in which our offices function, the way in which our cities work.
The way, you know, the amount of time that we have for preparing food and eating it with our friends and relations, and what sort of foods are easily available to us as well, to actually change the environment to be more supportive, and address those structural factors that are really driving these high rates of obesity and weight loss.
Alexis Pedrick: The jury is still out on whether Ozempic’s journey will end the same way that it ended for other weight loss drugs. The standard seems to be, does it work and not kill us? And so far, the answer is yes. So far. They’re still at the beginning of their drug journey.
Distillations is produced by the Science History Institute. Our executive producer is Mariel Carr. Our producer is Rigoberto Hernandez. And our associate producer is Sarah Kaplan. This episode was reported by Rigoberto Hernandez and mixed by Jonathan Pfeffer who also composed the theme music.
You can find all our podcasts, as well as videos and articles at sciencehistory.org/stories. And you can follow the Science History Institute on Facebook, Twitter, and Instagram for news about our podcast and everything else going on in our free museum and library.
For Distillations, I’m Alexis Pedrick. Thanks for listening.