Second-grader Randy Kerr begged to be first in line, as he so often did in his McLean, Virginia, elementary school. He held still for the doctor, and as the needle slipped into his arm and the cameras flashed, he put on a brave smile.
Under other circumstances a vaccination at school would have been no big deal. But the long-awaited vaccine Kerr received on that spring day in 1954 promised to protect him and his classmates from the most dreaded disease of the time: polio. And the clinical trial in which they were participating, along with 1.3 million other children across the country, promised to be the biggest medical experiment in history.
Which it was. Briefly.
Just a few years later, scientists in the Soviet Union tested a newer, different polio vaccine on a scale so vast it made the American trial look modest in comparison. By the time the two trials were completed, the world had two effective polio vaccines, both of which are still used around the world today. The drugs sprang from a golden age of vaccine production that followed World War II, an age that coincided with increasing hostility and brinkmanship between the two superpowers.
This is the story of how, against the backdrop of the Cold War, the superpowers’ domestic concerns drove unprecedented global action in the fight against disease—and how each power’s struggles to defeat other scourges, namely, smallpox and malaria, ultimately led to the recognition that neither the United States nor the Soviet Union could isolate itself from the rest of the world.
The poliovirus attacks the nervous system and can paralyze its (often young) victims within a few short hours. The resulting paralysis might be temporary, permanent, or even fatal. In the mid-20th century a polio diagnosis could have meant months, years, or even a lifetime confined to an iron lung, a coffinlike contraption that let patients with paralyzed chest muscles breathe. Every parent prayed their child would escape this fate.
Polio was more frightening still for its tenacity. Throughout the 1940s polio infections returned year after year in ever greater numbers, even as improved living standards, antibiotics, and vaccines snuffed out other infectious diseases.
One of those disappearing diseases was smallpox, a viral infection that caused full-body eruptions of painful blisters, internal bleeding, and, in its most virulent form, death. Thanks in large part to a vaccine in use for more than a century, both the United States and the Soviet Union had very few cases of smallpox within their borders by the time World War II was over.
In fact, by the early 1950s, the incidence of smallpox was so low that an extraordinary idea began to take hold. Scientists, inspired by new global institutions founded in a postwar spirit of cooperation, reasoned that if the world’s nations coordinated their efforts, the smallpox vaccine might wipe the disease from the face of the earth.
In 1953 the Canadian director general of the newly founded World Health Organization (WHO) proposed exactly that. But the United States considered the project too expensive and complicated, and the Soviets said nothing, having left the WHO as an act of Cold War protest. Without the support of the world’s superpowers the proposal languished.
For both the United States and the Soviet Union smallpox simply wasn’t a public-health priority, especially when compared with the climbing rates of polio. Regular panics seized the United States as polio returned summer after summer. Unsure how to keep the disease at bay, towns closed swimming pools and movie theaters, canceled high-school graduations and festivals, and advised parents to keep their children at home, where they wouldn’t come into contact with others who might be carrying the disease.
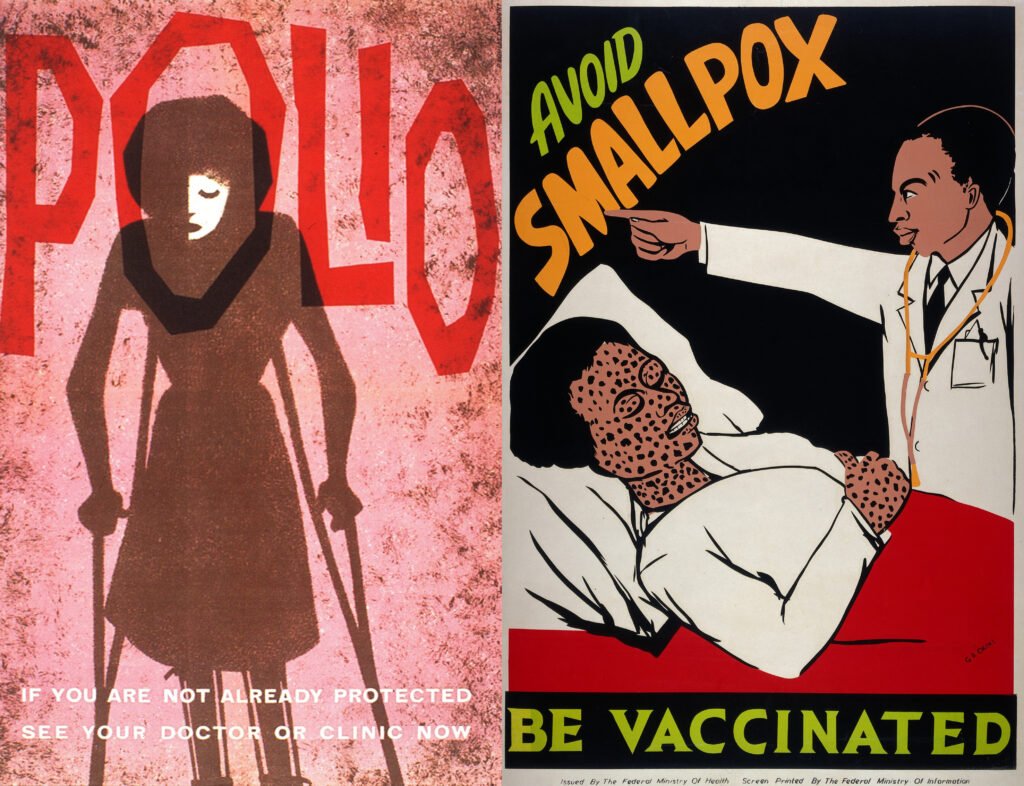
Public-health posters urging vaccinations for polio in Great Britain (left) and for smallpox in Nigeria (right).
In the Soviet Union polio’s existence had long been denied by Joseph Stalin. But after Stalin’s death in 1953 his successors decided that the nation’s recurrent polio epidemics could no longer be ignored. A vaccine or a cure was imperative.
By that time several American scientists were well on their way to developing an effective vaccine. In 1954 the University of Pittsburgh’s Jonas Salk announced that his vaccine was ready to be tested. It was Salk’s vaccine that Randy Kerr received in front of the banks of newspaper and television reporters in his school on that spring day in Virginia.
Salk’s injected vaccine was based on a controversial premise: he and his fellow researchers treated poliovirus with chemicals that killed it but left the remains recognizable to the immune system. The killed virus, they argued, would trick the immune system into thinking it was encountering live virus, which would prompt the body to manufacture disease-fighting antibodies. The problem with this approach, critics maintained, was the need to ensure that the virus in the vaccine was actually dead: otherwise the vaccine might cause polio, not prevent it.
One of Salk’s staunchest opponents was the University of Cincinnati scientist Albert Sabin, who was sure of the superiority of his own lab’s vaccine. Sabin’s vaccine contained live but weakened virus—a characteristic it shared with Louis Pasteur’s vaccine for the rabies virus. Moreover, Sabin’s vaccine wasn’t injected; it was swallowed, mimicking the way poliovirus itself entered the body. But Sabin’s vaccine wasn’t yet ready for testing.
A year after Kerr and his classmates were vaccinated, the Salk vaccine was declared effective. Across the relieved and grateful nation church bells pealed and sirens blared; schools and businesses stopped to observe a moment of silence. And Sabin continued to work on his vaccine.
While the Americans were vaccinating every child with the new Salk vaccine, the Soviets were getting their polio operations off the ground. In 1955 the Russians founded a Polio Research Institute in Moscow, headed by renowned virologist Mikhail P. Chumakov. One of the institute’s first missions was to gather as much information on polio prevention as possible. Given the success of the Salk vaccine, the United States seemed the obvious place to start—if not the easiest.
On a brisk January day in 1956 Chumakov left Moscow with fellow researchers Anatoli Smorodintsev and Marina Voroshilova (who was also Chumakov’s wife). The United States granted the Soviets permission to enter the country under strict supervision—and, for “security” reasons, under the condition that they travel only by train, despite their plans to visit labs across the country.
At the top of Chumakov’s list was a visit to Pittsburgh; after all, Salk’s vaccine had already been proven effective, and it was being used not only in the United States but around the globe. But in Cincinnati, in Sabin’s lab, Chumakov found something he wasn’t expecting: a friend. Although Sabin spoke little Russian and Chumakov little English, the two got on famously. Convinced that Sabin’s vaccine was worth pursuing, Chumakov invited Sabin to visit the Soviet Union. Sabin jumped at the chance.
Five months and two grueling FBI interrogations later, Sabin departed for Moscow. He spent the month of June 1956 giving lectures, meeting with researchers, and, according to historian David Oshinsky, “lobbying nonstop for his vaccine.” The Soviet Union had a decision to make between adopting the Salk or the Sabin vaccine, and Sabin pushed hard for his own.
On his return to Cincinnati, Sabin wrote to the State Department for permission to ship some of his virus samples to the Soviets. Despite Department of Defense warnings that the samples could be turned into biological weapons, the State Department approved. It was a move that may very well have sealed the vaccine’s fate.
A scientific battle still brewed over which vaccine embodied the better approach. Sabin later wrote that American virologists were telling him to toss his vaccine “in the sewer”—even though the WHO was calling for large-scale trials of live-virus vaccines. Sabin’s vaccine was now ready for testing, but with so many Americans already injected with Salk’s, there simply wasn’t an available test population in the United States. Unvaccinated Russians represented an opportunity that just didn’t exist at home.
In 1958 Chumakov tested a vaccine made with Sabin’s seed virus on 20,000 children. Emboldened by the results—the vaccine appeared safe, easy to administer, and effective—he decided to test it on an even bigger scale.
“We would very much want you to visit Moscow again in the Spring of 1959 to take part in the advancement of your vaccine,” Chumakov wrote to Sabin. “Will you agree to come?”
“I went,” Sabin later wrote, “and saw work on a scale that would have been impossible in the U.S.A. or elsewhere.”
With a single call to the head of public health at the Politburo, Chumakov put himself in charge of distributing Sabin’s vaccine to more than 15 million people in Soviet schools, hospitals, clinics, and nurseries before the year’s end. By the end of 1960 an additional 77 million children in the Soviet Union and another 23 million in East Germany, Czechoslovakia, Hungary, Romania, and Bulgaria all received the vaccine.
This wasn’t an experiment in the Western tradition; the Soviets employed neither control groups nor placebos, nor did they monitor children purposely denied the vaccine in order to compare their disease rates with those in vaccinated children, as had been done in the Salk trial. At the end of 1960 Chumakov wrote to Sabin that his vaccine was “winning new victories in our country.” Sabin was certainly glad to hear the news, but he knew the results would be rejected back in the United States.
He was right. The WHO dispatched its own independent expert, Yale University biologist Dorothy Horstmann, to verify the results. She penned a rather noncommittal report, saying that while the vaccine seemed to be working, definitive results would be a long way off. When the Soviets later sent a group of scientists to share their findings at the Second International Conference on Live Poliovirus Vaccines in Washington, D.C., the scientists found their work dismissed and belittled by the Americans.
It was just too much for the Soviet deputy minister of health, who cut off the attacks with a line that would be quoted decades later in scientific circles as a reminder that fundamental human needs ought to transcend political and cultural divides.
“I would like to assure [you] . . . that we in the Soviet Union love our children and are as concerned for their well being as much as people in the United States or any other part of the world are for their children,” said the minister.
In the meantime the Soviets had decided to rejoin the WHO—in part to press member nations to support the eradication of smallpox, as the WHO’s director general had first proposed back in 1953.
Both the United States and the Soviet Union were smallpox free by the mid-1950s, except for isolated cases that entered from beyond their borders. In the Soviet Union the infected came from Asia, bringing with them the anxiety and expense that accompanied possible epidemics. In the United States the last smallpox outbreak had happened in 1947, but the country was still spending $15 million to $20 million a year to vaccinate the population and keep the disease at bay.
The Russians were convinced this was a burden no advanced nation should tolerate. The proposal was as selfish as it was altruistic; if smallpox didn’t exist in poorer or less powerful nations, it wouldn’t find its way into more powerful ones. At the 1959 meeting of the WHO’s World Health Assembly in Minneapolis, Soviet Deputy Minister of Health Viktor Zhdanov presented a five-year plan for worldwide smallpox eradication and pledged that the Soviets would donate 25 million doses of vaccine to the cause.
This time around, the WHO’s member countries voted in favor of the proposal. The vote was, according to historian Nancy Leys Stepan, “a gesture of cooperation in the otherwise tense Cold War stand-off between the Western and the Eastern bloc countries.”
But if it was a gesture, it was a largely empty one. For the next several years the smallpox eradication effort—which the Americans never supported—was starved for funds and staff. The program’s office at WHO headquarters in Geneva was manned by a single physician and a single secretary. In the meantime the WHO project that the United States had enthusiastically endorsed—global eradication of malaria with the help of the cheap and easily administered new pesticide DDT—swallowed up the lion’s share of WHO resources to the tremendous annoyance of the Soviets.
In 1966, however, the United States did an about-face. Malaria eradication was failing, and smallpox, long gone from the United States, had recently made it past the nation’s borders. A smallpox-infected boy from Brazil had arrived in New York by plane and then boarded a train to Toronto, sending the whole northeastern seaboard into a panic. Not long after, a woman from Ghana checked into a Washington, D.C., hospital with smallpox, forcing the city to marshal all of its resources to track down her contacts and vaccinate every one. The woman, it turned out, did not have smallpox, but the lesson was clear: until smallpox was eliminated abroad, the country would have to deal with it at home.
In response a conflicted State Department—not wanting to give the impression of cooperation with their Cold War rival but wanting to put an end to smallpox—gave U.S. delegates to the WHO complicated instructions: they were to support a smallpox-eradication budget but not openly support eradication. As a result, by the end of the year the Soviets’ proposed project finally had the resources it needed, and the global smallpox eradication campaign got under way.
American scientists, later dubbed “smallpox warriors,” quickly assumed positions of leadership in the eradication campaign, which ensured that everyone exposed to smallpox worldwide was vaccinated until the disease had no one left to infect.
In short the United States ended up at the helm of an endeavor originally championed by their Soviet rivals, one that eliminated smallpox from all of humankind by the end of the 1970s. It was, in the words of D. A. Henderson, who led the vaccination campaign, a rare “Cold War victory.”
The eradication of smallpox inspired a global effort to eradicate polio in the 1980s. And the effects of the Cold War rippled through still other vaccination campaigns. First approved for sale in the United States in 1967, the mumps vaccine met with little enthusiasm among parents, doctors, and public-health experts—until it was revealed that the Soviets had already vaccinated more than a million youngsters against mumps. If there was a race to immunological power, it seemed the Soviets were winning. Soviet progress was one small but not inconsequential factor in the eventual acceptance of universal mumps vaccination in the United States.
The influence of the Soviet mumps vaccine is almost never mentioned in commonly told histories of mumps. And in the oft-repeated histories of smallpox eradication, Soviet-U.S. tensions are often reduced to a bit part.
Today, both Sabin’s and Salk’s polio vaccines support the ongoing global effort to eliminate the disease, which has been driven out of all but a handful of countries. In poorer countries where the risk for polio is still relatively high, Sabin’s is the vaccine of choice because it is cheap and easy to administer and because it “passively immunizes” other members of the community when it passes through the digestive system.
Sabin’s vaccine also carries a small risk for paralysis, however; so in countries where polio has already been eliminated, Salk’s is preferred. In the fullness of time it has proven to be safer. But both vaccines remain in use, relics of a long-ago immunological battle between two superpowers.